Jeremy, a four year old boy, had a good time playing in the park with his friends that sunny September day. A short time later, he came down with the common cold and, for a few days, had a runny nose and a slight cough.
When his mother entered his room the next morning to awaken him, she hoped the cold would be better. But Mom was shocked to discover he could not move his right arm. She called the child’s Pediatrician and was told to come to the office immediately. It seemed it took forever to arrive at the doctor’s office.
After a complete examination of Jeremy, the Pediatrician said, “I think he has Acute Flaccid Myelitis.”
“What is that?”
‘We suspect AFM is a viral infection that affects the spinal cord of the nervous system. It’ a polio-like condition — it’s not polio. This condition targets the gray matter of the spinal cord; the part concerned with movement of the limbs. It comes on suddenly causing muscles of the arms or legs to become flaccid meaning weak and limp“.
“My son can’t move his arm! It’s paralyzed!” How did this happen?“
“We just don’t know how Jeremy or other children get this frightening condition. We haven’t identified the exact cause of AFM — why it happens or if some children are more likely to get it compared to other children. We think viruses may be causing the paralysis but we don’t know for sure.”
What about treatment for my son?“
“I’m sorry but we don’t have good treatments for this problem and one reason is that we don’t know what causes AFM. Some children with this condition recover quickly while others require ongoing care. Careful follow up, physical therapy and surgery have been helpful for children with this problem.”
“What surgery?”
“Surgeons have transposed a nerve from the rib cage to the arm and have had some success with this procedure. Right now, I recommend Jeremy have a few tests done to confirm my diagnosis.”
The Center for Disease Control and Prevention (CDC) has confirmed 300-400 case of AFM since 2014. Sixty two of the cases so far have been confirmed in 2018 occurring in 22 states.
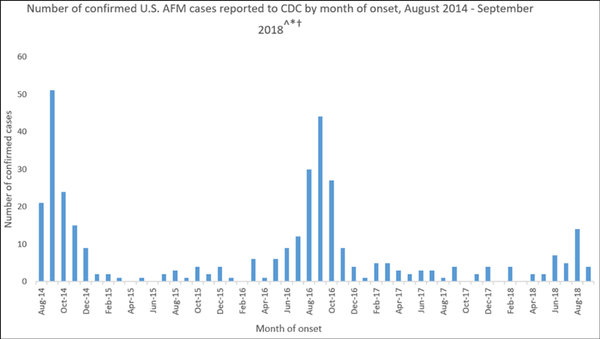
Source: CDC Number of cases of AFM from 2014 to 2018
A respiratory virus, enterovirus-EV D68, has been identified in several children with AFM, but more evidence is needed to conclude that this is the sole cause of this condition.
Acute flaccid myelitis is described as polio-like because doctors think it may be a viral infection affecting the motor nerve of the spinal cord the way polio did. Characteristically the arms and legs of children are weak with a loss of muscle tone and reflexes.
Besides limb weakness, some children experience difficulty moving the eyes, drooping eyelids, facial weakness, trouble swallowing or slurred speech. Nine out of ten cases of AFM are in children 18 years of age and younger. It occurs most often in children of about 4 years of age.
Clusters of AFM typically spike in September and October. The diagnosis is confirmed after doing a spinal tap and a MRI of the spinal cord in children with limb paralysis.
Parents are urged to keep your child up to date on immunizations. They’re asked to encourage their child to do common sense things such as to cough into the elbow of the
arm and wash their hands frequently.
AFP is a rare condition, but the aftershocks are devastating to parent and child. The CDC has warned that in 2018 AFM is on the rise in the United States. Parents are urged to seek medical assistance as soon as possible if your child has any of the symptoms noted above. As one infectious disease doctor said when his son got sick in autumn of this year: “I hope it’s just a cold.”
References
- Transcript for CDC; Telebriefing: Update on Acute Flaccid Myelitis; October 17, 2018
- CDC, Acute Flaccid Myelitis; October 22, 2018
- Queensland Health; Acute Flaccid Myelitis; August 10, 2017
- American Academy of Pediatrics; Acute Flaccid Myelitis; 2018
This article is intended solely as a learning experience. Please consult your physician for diagnostic and treatment options.
